When Hospitals Shrink: Preventing Loss of Hospital Beds Through Effective Bed Management
- In ICU
- Fri, 19 Apr 2024
With an ageing population and more sophisticated treatments, hospitals must become more bed-efficient or risk contracting. Strategic management is needed since ineffective bed management can reduce bed availability.
Introduction
There are multiple challenges for healthcare institutions in the coming decades. Important demographic changes are taking place in most countries in the world, demonstrating a progressive ageing of the population. By 2030, 1 in 6 people in the world will be aged 60 or over. This portion of the population will increase from 1 billion in 2020 to 1.4 billion. By 2050, it will double (2.1 billion). The number of people aged 80 and over is expected to triple between 2020 and 2050, reaching 426 million. Even though it is believed that this process is inherent to developed countries, the fact is that in 2050, two-thirds of people aged 60 or over will be in poor or developing countries (WHO 2022). Worldwide, there has been an increase in life expectancy, with a global average of 73 years in 2023 (WHO n.d.),reaching more than 80 years in some developed countries. A greater prevalence of chronic diseases leads to a greater number of medical consultations in emergency rooms, as well as admissions. Patients aged 65 or over accounted for 32.7% of medical consultations in the United States in 2018, although they account for approximately 16.7% of the American population (CDC 2021). These patients are also those who remain in the hospital for longer periods, as they are physically fragile. The need for beds is becoming increasingly greater, and healthcare institutions are increasingly under pressure to meet this demand. In Brazil, many hospitals work with high occupancy rates (Power360 2022), making increasingly efficient bed management necessary.
Hospital Bed Management Must Be Proactive, Not Reactive
Increasingly, hospital bed management (HBM) is seen as a marker of quality. Purely reactive responses to demands must be a thing of the past, making it necessary to search for an adequate turnover of hospital beds constantly proactively. Many institutions, however, have difficulties in unifying efforts between sectors, which have an interdependent relationship. An adequate HBM in one or two sectors of the hospital will have little effect if it is not replicated in other areas. Most sectors function as receivers and suppliers of patients in relation to the other, with one role or the other predominating. The Intensive Care Unit (ICU), for example, is responsible for receiving critically ill patients from all sectors of the hospital. Given the reality of a lack of beds for critically ill patients in Brazil and around the world, the beds in these units become especially valuable, both from an institutional and regional point of view, as it is not uncommon for patients to be transferred between hospital units in search of this type of support. Within the hospital, patients in the emergency room and infirmary are constant candidates to occupy an ICU bed (Figure 1). Therefore, it is very important that patients are discharged as soon as they are clinically fit to do so, freeing up space for more seriously ill patients.
On the other hand, the lack of turnover in ward beds can also compromise the ICU as it is the main destination for discharged patients (Figure 2).
Intermediate care units, surgical centres, and emergency rooms (ER) are also interdependent, as they send and receive patients from all sectors (Figures 3, 4 and 5).
The ER is particularly sensitive and prone to inadvertently accumulating patients, as it depends heavily on other sectors to rotate its beds. Instilling a proactive HBM culture, with responsibilities and duties for employees, is very important so that there is no backlog of patients in the most varied sectors.
A microsystemic view may predominate in a certain area of the hospital, generating a negative impact on all others, as it is not uncommon for professionals in a certain sector to underestimate the institutional impact of their decisions.
Barriers to Adequate Hospital Bed Turnover
There are many barriers to achieving an adequate turnover of hospital beds (Table 1). Among them, one that attracts the most attention is the lack of transparency regarding the beds available in the hospital. The value of a hospital bed is very high, especially when it comes to public health, and therefore, this is a resource that must be managed in the most transparent way possible. There should be no major bureaucracy so that nurses and doctors can access an electronic map of hospital beds, which shows which are available and in which sectors. The electronic system must replace other less efficient methods, such as telephone calls between sectors. Furthermore, each hospital must have a section responsible for managing the flow of patients and allocating them to the part of the hospital best suited to their needs, according to the severity and risks involved. To this end, it is necessary to establish criteria for admission to infirmary and ICU beds. In the United States and Canada, this section is colloquially called "bed flow" and is generally composed of nurses responsible for the institution's HBM. At a more advanced stage of bed management, it will be possible to view not only the institution's beds but also those of other hospitals in the region, allowing for more efficient regional regulation. Some Brazilian hospitals in the Unified Health System (SUS- Sistema Único de Saúde) have an Internal Regulation Center (NIR- Núcleo de Regulação Interna) (Ministério Da Saúde 2017), responsible not only for internal bed management but also for contacting the Health Service Offers Regulation Center (CROSS- Central de Regulação de Ofertas de Serviços de Saúde) (Alesp 2016). Through CROSS, it is possible to obtain resources not available in a specific hospital unit, such as ICU beds, consultations with a medical specialty, and laboratory or imaging tests.
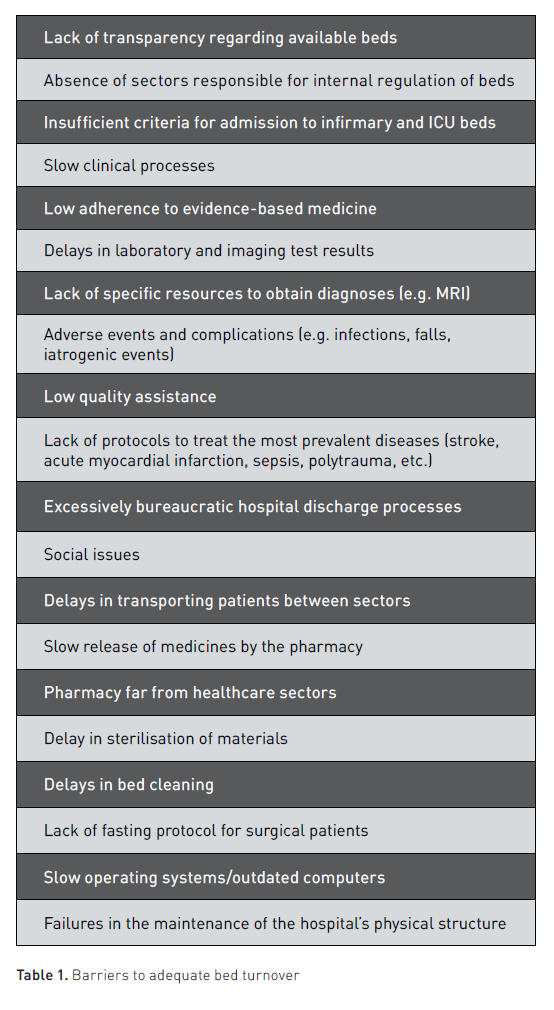
Delays in obtaining a suitable bed contribute to another problem, which is the delay in starting medical care. Slow clinical processes are an important source of delays in the discharge and bed turnover process. Low adherence to evidence-based medicine delays clinical recovery, highlighting the importance of clinical leadership. Other frequent causes are the delay in test results or the lack of specific resources to obtain diagnoses, such as an MRI exam. It is also worth highlighting the occurrence of preventable adverse events, such as falls or infections associated with low-quality care. The lack of protocols for treating the main pathologies treated in the hospital environment, such as stroke, acute coronary syndrome, urinary tract infection, community-acquired pneumonia, and sepsis, among others, increases the morbidity and mortality of these diseases and the length of stay in hospital. It is also important to have other protocols: to avoid bronchoaspiration, prophylaxis of venous thromboembolism and stress ulcers, patient disinvasion, oral hygiene, weaning of mechanical ventilation and oxygen use, intravenous contrast injection, use of vasoactive drugs, precaution contact and isolation, palliative care, heparinisation, glycaemic control, analgesia and sedation and haemodynamic monitoring. The idea is that there is prophylaxis of common complications in the hospital environment, which are factors that increase the length of stay. Other protocols seek to speed up the removal of medications and devices that cause complications when they remain in the patient for an unnecessary time, such as vasoactive drugs, analgesia and sedation, venous catheters, and supplemental oxygen.
Slow bureaucratic discharge processes also constitute a considerable barrier. Prioritising medical discharge during the clinical visit in the morning should be a priority for the service, preferably by 10 am. When medical discharge occurs early, it becomes easier for the family to organise themselves to remove the patient from the institution. Medical discharge efforts begin when the patient is admitted to the hospital and include the preparation and dissemination of a booklet for families guiding the discharge process and providing instructions regarding schedules, means of transportation and medical advice. The expected day of discharge must be widely publicised among family members and staff so that there is a certainty that all issues have been adequately addressed, such as pending exams, medications for continuous use and instructions for home. It should be noted that most of the time, the failure to meet the expected discharge date is related to family issues, and therefore, opportunities to guide the patient's family are important. Social cases in which the family claims to be unable to care for the patient must receive special attention, as they often result in very prolonged hospitalisations.
The Role of the Clinical Leader in the Bed Management Process
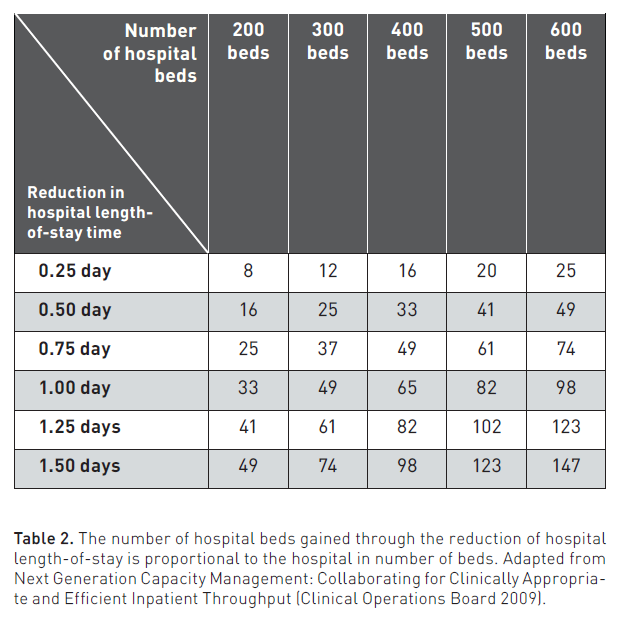
A gain of a few hours in the patient discharge process has a significant impact on the number of effective beds in a hospital. A 6-hour reduction in the average length of stay for patients in a 300-bed hospital is similar to adding 12 beds to the institution (Table 2). If the average length of stay is reduced by one day, the impact is similar to the addition of 49 beds in the hospital (Clinical Operations Board Advisory Board International 2009).
There is no doubt that the role of the clinical leader becomes important, as it will implement evidence-based medicine, seeking to streamline clinical processes. Each sector of the hospital must have a medical leader responsible for seeking answers to the following questions pertinent to each patient: (1) what is the patient's clinical status? (2) what is the patient's functional status? (3) what is the goal to be achieved for the patient's discharge? (4) what is the plan and goal to be achieved today? (5) what is the expected date of hospital discharge? Discharge efforts begin at the time of admission; therefore, such questions should be asked from the first day of hospitalisation.
Associating a management vision with clinical care is a differentiating factor for good clinical leaders and is not something that is actively taught in most medical schools. This managerial and proactive vision regarding HBM is much more integrated with nursing than with doctors (Soares et al. 2016). It is urgent that notions of hospital management are part of the medical curriculum, associated with better knowledge in urgency and emergency, in addition to intensive care. The clinician who makes the biggest difference in the hospital environment is the one who knows how to recognise and act in high-risk situations for the patient, which in itself is already a challenge. However, it is necessary to go further: the doctor needs to have a comprehensive view of the functioning of the hospital and how his actions impact its functioning. Poor management of hospital beds "shrinks" the hospital, reducing the number of beds available to the population. The responsibility for an adequate HBM lies with everyone who works in the institution, from employees linked to bureaucracy to those who process and carry out exams to professionals linked to assistance. A good clinical leader will lead these processes.
It is necessary for discharge but with safety and quality. Precipitous hospital discharges increase hospital readmission rates and worsen the view that the population and professionals have of the institution. In the ICU, hasty discharges also increase the rate of readmission to the unit, in addition to increasing mortality and the risk of events such as falls and cardiorespiratory arrests in the ward.
Other Bottlenecks That Increase Hospital Stay
Ancillary services support general hospital operations but are not directly related to patient care. We can cite as examples the laboratory, radiology service, pharmacy, nutrition, social services, cleaning, sterilisation of materials, maintenance and IT services (Information Technology). Delays in releasing laboratory results can significantly delay a patient's discharge, as well as lead to errors in the treatment of the patient's pathology.
In relation to radiology, much of the efficiency of this sector is related to the speed at which reports of the exams are released. Even if there are no doctors available to discuss or release reports, ideally, they should be released remotely online. It is important to emphasise that the radiology service also depends on the internal transport of patients so that they can be taken to their sector, as many exams, such as CT scans and MRIs, will not be carried out at the bedside.
The release of medicines by the pharmacy is also a relevant factor, and there are organisational details that make a difference. The pharmacy must be decentralised and close to the location it intends to serve, such as the ICU and emergency room. Each hospital unit has its own specific demand, which will be met by the pharmacy subunit in its sector. Maintaining a centralised service in a single pharmacy will result in employees having to travel long distances to obtain medications, delaying care and treatment.
Offering a diet to the patient has an impact on the length of stay, particularly in relation to post-operative patients. When recovering from major abdominal surgeries, acceptance of the prescribed diet and administration at the correct time is a factor in speeding up discharge, benefiting both the patient and the hospital. On the other hand, when a diet is inadvertently offered to patients who are fasting for surgery, the day of the procedure and the time in the operating room are lost, resulting in multiple losses. Failures in the material sterilisation service can also delay surgeries and other procedures due to a lack of sterile surgical drapes, gowns and surgical material.
Cleaning the beds is also part of the discharge process in the final phase. It is important that it begins without delay, aiming to make beds available early for new admissions. The cleaning team's response time, once called, must be less than 20 minutes, and the time actually spent cleaning the bed must be less than 40 minutes, with a total time of less than 1 hour (Brown and Kros 2010). Once completed, the time involved in transporting patients to their bed after admission must be assessed, which should not take more than 15 minutes. It is expected that the employee responsible for transporting patients will be able to carry out an average of 3 to 4 transports per hour.
Social cases in which the family claims to be unable to care for the patient must receive special attention, as they often result in very prolonged hospitalisations. There are cases in which hospitalisation lasts for years. A proactive social service is necessary to seek solutions for these patients, whether by actively contacting the family or helping them obtain resources that facilitate patient care.
Proper maintenance of equipment avoids delays due to machinery failures. The maintenance service will take care of this, as well as repairs to the hospital's physical structure, allowing the institution to operate at its full capacity. Failures in the hydraulic system, infiltrations, and malfunctions in the oxygen and vacuum systems are examples of problems that can render a bed or entire hospital wards unusable and must be prevented and resolved quickly.
The IT service resolves problems related to operating systems, such as electronic medical records, image viewing and laboratory exam systems, and internet network maintenance. Failures in any of these systems directly impact care and all hospital sectors. The lack of operation for just one day of any of them can generate chaos. Therefore, it is necessary to use contingency plans when problems arise so as not to freeze assistance activities. Manual filling forms must be available in order to alleviate the lack of electronic systems. Another problem related to IT that impacts the speed of processes is updating machinery, as outdated computers can make operating systems extremely slow or even lead to failures when using them. Hospitals with poor internet networks or obsolete machines often make it difficult for staff to complete electronic medical records. The impact of this obstacle should not be underestimated, as healthcare professionals usually spend up to 40% of their time in the hospital recording their care.
The Most Common Root Causes
In a systematic review of the causes of patients remaining in hospitals for a long time, Ahlin et al. (2022) listed process delays, insufficient capacity, inefficient coordination of available resources and high variability in capacity utilisation as the root causes of all barriers to adequate bed rotation.
The time taken to start or end an activity in the hospital, such as surgeries, diagnostic tests, sector transfers and test results, affects the time the patient remains in the hospital (Johnson et al. 2020). It takes time to start the discharge process for patients who are already able to being released is also an example of delay in processes.
Innovative management of hospital capacity and efficient processes will not always be able to resolve the fact that the hospital does not have enough beds or well-designed staff to deal with a given demand. In Brazil, it is common for both factors to be far from what is necessary. The lack of triage nurses, doctors, clerks, flow coordinators, pharmacists, and employees in the sectors responsible for exams is an important cause of delays. Lack of machinery is also a reason for wasted time in processes (for example, lack of available computers).
High variability in capacity utilisation is a factor that is independent of the service but can significantly impact bed turnover. The recent COVID-19 pandemic generated a major resource crisis, with many hospitals needing to make emergency hires and a spatial relocation of their sectors, notably the ICUs. Although the poor results in the treatment of intubated patients are closely related to a lack of human resources (Batista et al. 2022), the impact caused by the lack of physical space and equipment should not be underestimated. Several discussions about the real space that ICUs should occupy in hospitals were initiated, with arguments for and against the increase in these units (Valley and Noritomi 2020; de Lange et al. 2020; Phua et al. 2020). Modern hospitals must have flexible and adaptable bed sizing in the face of possible emergency situations. Unfortunately, recurring viral pandemics are a global reality (Cheng et al. 2007), and other emergencies will arise.
Use Of Indicators: Making a Diagnosis of Hospital Bed Turnover
Hospital Length of Stay
Hospital length of stay (HLS) is defined by the period that a patient remains in the hospital from the day of admission until discharge. A high proportion of patients remain in the hospital excessively, generating low productivity per bed. The health system has become increasingly competitive, and there is a growing demand for reducing hospital stays and care costs (Ministério Da Saúde 2013). Length of stay is a marker of bed turnover and, therefore, the number of patients treated in the hospital in a given period of time. The period of time covered must be longer than the length of stay; otherwise, there will be no bed turnover and turnover assessment. There are several ways to calculate this indicator.
In short-stay hospitals, the calculation must involve the number of hospital entries and exits and is done as follows:
HLS=(number of patients who were admitted in the period)/(number of patients who left the hospital in the same period)
Long-stay hospitals can be calculated as follows:
HLS= (sum of days of hospitalisation for each patient in the period)/(number of patients in the same period)
The interpretation of the results is important, and the type of procedure performed, the disease profile of the patients, and their social status must be taken into account. It will be up to the manager to carry out an adequate reading of the numbers, as a hospital in which many patients are hospitalised beyond the necessary time because they cannot obtain external resources quickly (for example, haemodialysis clinics, performing coronary angiography or obtaining heart surgery) will certainly have this indicator highly impacted by the delay. Patients with a fragile social situation in more impoverished areas also end up spending long periods hospitalised in health institutions, as they cannot find caregivers at home or are homeless.
Hospitals with an eminently surgical and low-complexity profile will have a shorter average length of stay than those in which the patients admitted are mostly clinical and highly complex, with multiple comorbidities. It should also be noted that the occurrence of in-hospital complications (such as nosocomial infections, falls, and other adverse events) also negatively impacts this metric, inadvertently expanding the length of stay. It can also be calculated in patient days as follows:
HLS=(number of patient-days in the period)/(number of departures in the period)
Patient-day is the unit of measurement representing the service or assistance offered to the patient who stayed overnight in the hospital. Therefore, the number of patient days will correspond to the number of patients staying overnight in the hospital each day. The final number of patient days in the month, for example, will be the sum of patient days for each day over the 30 days. To count departures, we must add the number of discharges, deaths, and external transfers that occurred in the hospital over that period of time. According to the National Supplementary Health Agency, in hospitals for acute patients, the average length of hospitalisation should be between 3 and 5 days, and it will be highly influenced by the complexity of the patients (age, number of comorbidities, severity, and complexity of resources necessary). Psychiatric and pulmonology hospitalisations tend to have a significant impact on these patients, as these patients are hospitalised for a prolonged period of time. Three large institutions on the outskirts of São Paulo and Salvador (Hospital Municipal de Cidade Tiradentes, Municipal Health Secretariat of Diadema and Hospital do Subúrbio de Salvador) presented between 2011 and 2012 a hospital length of stay estimated between 3.5 and 6.4 (Ministério Da Saúde 2013). In the Brazilian public health system, the delay in obtaining some medium and high-complexity resources, such as haemodialysis or heart surgery, ends up greatly increasing this indicator. It is not uncommon for patients to remain in hospitals for weeks due to the delay in obtaining these resources.
Occupancy rate
This is a fundamental indicator for evaluating the hospital’s turnover and service capacity (Ministério Da Saúde 2012). It can be applied to the hospital as a whole or to each sector individually, allowing a specific analysis of a given department. It is even possible to compare the value obtained for the entire institution with that of a sector, allowing adjustments in the number of beds according to demand. It is calculated by dividing the number of patients treated on a given day by the number of beds available on that same day, as described below:
Occupancy Rate = (number of patients occupying beds in one day)/(number of beds available in the same day) x 100
The result will be expressed as a percentage.
Patients who are under observation and who will be released quickly should not be taken into account. However, in the Brazilian reality, where several patients remain inadequately hospitalised in emergency beds that should be for observation, these patients must be included in the count, as they remain in the hospital for several days. The situation in public hospitals in Brazil shows a large number of patients on stretchers and other temporary beds, and these beds should not be included in the calculation as they are not official beds with adequate infrastructure, or a multidisciplinary team designed to care for these patients. Therefore, these institutions most likely also have fully occupied wards and Intensive Care Units, which would constitute an occupancy rate greater than 100%, compatible with the overcrowding they experience. As extra beds are not included in the calculation and patients are, there are more patients than beds.
On the other hand, if we have a certain sector with an occupancy rate of 50% and the hospital's general rate is 70%, it would be appropriate to resize beds and resources, reducing them for the sector with the lowest occupancy rate. However, it is necessary to assess whether this trend is confirmed in other periods of time (following days, weeks, or months). There is a seasonality in the occupancy rate and patient flow in emergency rooms, for example. School vacation periods tend to reduce the number of emergency room visits and, consequently, the number of hospitalisations. On the other hand, viral pandemics such as COVID-19 can greatly increase this same flow in the opposite direction. It is necessary to take this data into consideration when resizing.
Return on Investment
Return On Investment (ROI) is a calculation that will quantify how much a given investment was worth within the context of the hospital (AHRQ). For example, if the hospital carries out an expansion process, aiming for an increase in revenue, the ROI will be able to assess whether the cost-benefit ratio of the investment was good or not. It is possible to apply this calculation to procedures performed on patients, care provided by healthcare professionals, profitability of departments, or the implementation of protocols and educational measures. The idea is to calculate how much each of these interventions generated in expenditure and return for the institution as follows:
ROI= (revenue - initial investment )/(initial investment)
ROI, for example, can be decisive in the evaluation of a renovation in a certain sector of the hospital, with the aim of increasing the number of visits and revenue. However, it must be interpreted according to the period of time in which it was applied. Revenue may be low initially but increase over a longer period of time. Alluding to the purchase of equipment, a new tomography device can present a negative ROI in the first month but evolve into a highly positive metric over the course of one year. This indicator can be applied to almost any intervention, such as hiring new professionals or meeting new health insurance plans at the hospital.
Average Length of Stay in the Emergency Room (ALSER)
It is the measurement of the average time, in hours, spent in the emergency department of patients admitted to this sector, from the time of arrival until the end of care. It can be calculated by the following formula:
ALSER=(∑the length of stay of each patient treated in the emergency in that period)/(number of visits to the emergency in that period)
The length of stay in the emergency room must be optimised to avoid excessive patients in this sector. In general, the stay of patients for prolonged periods in the emergency department is associated with worse outcomes, especially when dealing with patients with organic dysfunctions (Machado et al. 2023). Emergency, in general, does not have professionals accustomed to the continuous management of critically ill patients or even trained in the clinical management of complex cases. It also does not have appropriate resources to adequately monitor critically ill patients in most cases due to a lack of adequate machinery and beds. Therefore, it is not recommended that patients remain in the emergency room for long periods and should be directed to hospitalisation units with adequate support for the case, such as wards and ICUs.
In Brazil, unfortunately, it is common to see a large number of patients admitted to the emergency room, mainly in the Brazilian public health system. The causes for this inadequacy are many, from the hospital's lack of efficiency in releasing hospital discharges to the lack of beds to meet the demand imposed by a large population in need of care. When we think about the reality of Brazilian hospitals, ICU beds are scarce, which makes the flow of patients in the hospital extremely difficult, especially in the emergency room. However, there is also often a lack of trained professionals to care for critically ill patients, which undoubtedly favours the worsening of outcomes and the occurrence of delays in the turnover of beds in the units. A study carried out by the Federal Court of Auditors (Tribunal de Contas da União) in 2014 showed that the overcrowding of hospitals in Brazil is a reality for the majority of hospitals (Matoso 2014). This fact leads to an overload of work for the professionals involved in emergency room care and even worse outcomes.
The Inefficient Surgical Centre
Contrary to what many people imagine, the surgical centre is not always a source of profit for hospitals. There is often a poor dimensioning of the sector, which has excessive rooms to meet peak needs, but in practice, they remain idle for too long (Business & Health Consultoria e Auditoria em Saúde). Inadequate management of the surgical schedule can end up increasing this idleness, as well as the number of cancellations. Operating room reservations, which often wait hours for the most renowned surgeons, accumulate delays and only increase this loss. Delays in cleaning and preparing beds for the next procedure are other sources of losses. A survey in 2021 (Medicina S/A) estimated the average cost/hour of the surgical centre of 112 hospitals at 783 BRL, and this value tends to increase, given the high fixed costs associated with the growing technology involved in the procedures.
The Future: Use of Artificial Intelligence in Hospital Bed Management
The use of artificial intelligence in hospitals is already a reality. Medical decision support programmes already exist and allow professionals to make diagnoses and take actions more based on scientific evidence (Magrabi et al. 2019). In the near future, it is expected that a large part of medical decisions will be assisted by artificial intelligence (Filho 2021), including the discharge process. Through a machine learning process, data relating to the patient will be crossed, including vital signs (Rush et al. 2019), laboratory tests, and image exams, allowing the programme to suggest the correct time for hospital discharge (van de Sande et al. 2022). At a more advanced stage, this discharge will enter the hospital bed management system, and the programme itself will manage beds intelligently, according to the demands existing at that time. This way, time will be saved, avoiding possible losses both at the time of discharge and in bed management. The use of algorithms will allow automation and consequent acceleration of processes by incorporating protocols established by human beings. Programmes will even be able to estimate the number of beds needed in certain sectors of the hospital to meet demands (Ortiz-Barrios et al. 2023). Some algorithms are already in the validation phase and will very soon be incorporated into daily practice. Nexar Flow (Nexar Systems), for example, is under development to facilitate the transfer of care in an automated way, increasing the efficiency of clinical processes.
Conclusion
HBM is an important marker of quality in the management of healthcare institutions and a fundamental part of their functioning. Its importance will grow increasingly in the coming decades, and the use of artificial intelligence will facilitate this task, being inexorably incorporated into management. There are many challenges for clinical staff in the years to come, as it will be necessary to incorporate management notions into the institutions' clinical leadership, as well as some proficiency in handling automated algorithms for clinical practice.
Conflict of Interest
None.
«« Navigating the Implementation of AI in Intensive Care Medicine
Artificial Intelligence in Critical Care: Opportunities and Obstacles »»
References:
CDC (2021) Visits to physician offices and hospital emergency departments, by age, sex, and race: United States, selected years 2000–2018. Available at https://www.cdc.gov/nchs/data/hus/2020-2021/HCareVis.pdf
Åhlin P, Almström P, Wänström C (2022) When patients get stuck: A systematic literature review on throughput barriers in hospital-wide patient processes. Health Policy. 126(2):87-98.
Alesp (2016) Law sanctioned that guarantees scheduling of consultations and exams through the CROSS system. Available at https://www.al.sp.gov.br/noticia/?id=372943#:~:text=A%20Central%20de%20Regula%C3%A7%C3%A3o%20de,2%20de%20agosto%20de%202010
Brown EC, Kros J (2010) Reducing room turnaround time at a regional hospital. Qual Manag Health Care. 19(1):90-102.
Business & Health Consultoria e Auditoria em Saúde (n.d.)The idle capacity of surgical centers is 62%, according to research. Available at https://www.businessinhealthconsultoria.com/noticia/a-ociosidade-dos-centros-cirurgicos-e-de-62-informa-pesquisa#:~:text=As%20palavras%20de%20ordem%20quando,em%20sa%C3%BAde%20s%C3%A3o%3A%20evitar%20desperd%C3%ADcio
Cheng VC, Lau SK, Woo PC, Yuen KY (2007) Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection. Clin Microbiol Rev. 20(4):660-94.
de Lange DW, Soares M, Pilcher D (2020) ICU beds: less is more? No. Intensive Care Med. 46(8):1597-1599.
Filho LACB, Randhawa VK, Maciel AT, Coimbra MR (2022) We need to talk about critical care in Brazil. Clinics (Sao Paulo). 77:100096.
Filho LACB (2021) Artificial intelligence: what should an intensivist have in mind in the beginning of the new era. Anaesth Pain intensive care. 25(1):8-12.
Johnson M, Burgess N, Sethi S (2022) Temporal pacing of outcomes for improving patient flow: design science research in a National Health Service hospital. J Oper Manag.
Machado FR, Cavalcanti AB, Braga MA et al. (2023) Sepsis in Brazilian emergency departments: a prospective multicenter observational study. Intern Emerg Med. 2023 18(2):409-421.
Magrabi F, Ammenwerth E, McNair JB et al. (2019) Artificial Intelligence in Clinical Decision Support: Challenges for Evaluating AI and Practical Implications. Yearb Med Inform. 28(1):128-134.
Matosa F (2014) TCU points to permanent capacity in 64% of hospitals and emergency rooms. Available at https://g1.globo.com/bemestar/noticia/2014/03/tcu-aponta-lotacao-permanente-em-64-dos-hospitais-e-prontos-socorros.html.
Média de Permanência Geral (2013) Ministério da Saúde e Agência de Saúde Suplementar. Available at https://www.gov.br/ans/pt-br/arquivos/assuntos/prestadores/qualiss-programa-de-qualificacao-dos-prestadores-de-servicos-de-saude-1/versao-anterior-do-qualiss/e-efi-05.pdf
Medicina S/A (2021) Survey: average cost/hour of surgical centers is R$783. Available at https://medicinasa.com.br/custo-centro-cirurgico/.
Ministério Da Saúde (2017) Manual de Implantação e Implementação- NIR Available at https://www.cosemssp.org.br/wp-content/uploads/2021/04/Manual_NIR.pdf
Nexar Systems. Nexar Flow: Management of care transfers for the 21st Century. Available at https://nexar.systems/hsl/
Next-Generation Capacity Management: Collaborating for Clinically Appropriate and Efficient Inpatient Throughput (2009) Clinical Operations Board Book. First Edition.
Occupancy in hospitals exceeds pre-pandemic levels, says ANS (2022) Available at https://www.poder360.com.br/saude/ocupacao-em-hospitais-supera-nivel-pre-pandemia-diz-ans/
Ortiz-Barrios M, Arias-Fonseca S, Ishizaka A et al. (2023) Artificial intelligence and discrete-event simulation for capacity management of intensive care units during the Covid-19 pandemic: A case study. J Bus Res. 160:113806.
Phua J, Hashmi M, Haniffa R (2020) ICU beds: less is more? Not sure. Intensive Care Med. 46(8):1600-1602.
Return on Investment Estimation. Agency for Healthcare Research and Quality. Available at https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/systems/hospital/qitoolkit/combined/f1_combo_returnoninvestment.pdf
Rush B, Celi LA, Stone DJ (2019) Applying machine learning to continuously monitored physiological data. J Clin Monit Comput. 33(5):887-893.
Soares MI, Camelo SH, Resck ZM, Terra Fde S (2016) Nurses' managerial knowledge in the hospital setting. Rev Bras Enferm. 69(4):676-83.
Taxa de Ocupação Operacional Geral (2012) Ministério da Saúde e Agência Nacional de Saúde Suplementar. Available at https://www.gov.br/ans/pt-br/arquivos/assuntos/prestadores/qualiss-programa-de-qualificacao-dos-prestadores-de-servicos-de-saude-1/versao-anterior-do-qualiss/e-efi-01.pdf
Valley TS, Noritomi DT (2020) ICU beds: less is more? Yes. Intensive Care Med. 46(8):1594-1596.
van de Sande D, van Genderen ME, Verhoef C et al. (2022) Optimizing discharge after major surgery using an artificial intelligence-based decision support tool (DESIRE): An external validation study. Surgery. 172(2):663-669.
World Health Organization (2022) Ageing and Health. Available at https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
World Health Organization (n.d) Life expectancy at birth (years). Available at https://www.who.int/data/gho/data/indicators/indicator-details/GHO/life-expectancy-at-birth-(years)