Perspective > Medscape > Fast Five Quizzes
Fast Five Quiz: Refresh Your Knowledge on Key Aspects of Sepsis
Richard H. Sinert, DO
June 07, 2018
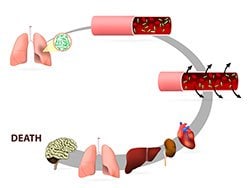
Sepsis is defined as life-threatening organ dysfunction due to dysregulated host response to infection. Organ dysfunction is defined as an acute change in total Sequential Organ Failure Assessment (SOFA) score greater than 2 points secondary to the infection cause. Septic shock occurs in a subset of patients with sepsis and comprises an underlying circulatory and cellular/metabolic abnormality that is associated with increased mortality. Septic shock is defined by persisting hypotension that requires vasopressors to maintain a mean arterial pressure of 65 mm Hg or higher and a serum lactate level greater than 2 mmol/L (18 mg/dL) despite adequate volume resuscitation.
Detrimental host responses to infection occupy a continuum that ranges from sepsis to severe sepsis to septic shock and multiple organ dysfunction syndrome (MODS). The specific clinical features depend on where the patient falls on that continuum. Patients with sepsis may present in a myriad of ways, and a high index of clinical suspicion is necessary to identify subtle presentations.
Do you know important attributes of sepsis presentation, diagnosis, and treatment? Test your knowledge with this quick quiz.
Q1: Which of the following is accurate about the etiology and epidemiology of sepsis?
A1: Risk factors for sepsis and septic shock include extremes of age (<10 years, >70 years) and underlying genetic susceptibility
 Risk factors for severe sepsis and septic shock include the following:
Risk factors for severe sepsis and septic shock include the following:
- Extremes of age (<10 years and >70 years)
- Primary diseases (eg, liver cirrhosis, alcoholism, diabetes, cardiopulmonary diseases, solid malignancy, and hematologic malignancy)
- Immunosuppression (eg, from neutropenia, immunosuppressive therapy [eg, in organ and bone marrow transplant recipients], corticosteroid therapy, injection or intravenous drug use, complement deficiencies, asplenia)
- Major surgery, trauma, or burns
- Invasive procedures (eg, placement of catheters, intravascular devices, prosthetic devices, hemodialysis and peritoneal dialysis catheters, or endotracheal tubes)
- Previous antibiotic treatment
- Prolonged hospitalization
- Underlying genetic susceptibility
- Other factors (eg, childbirth, abortion, and malnutrition)
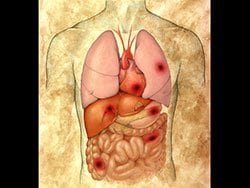
In the more common form of MODS, the lungs are the predominant, and often the only, organ system affected until very late in the disease. Patients with this form of MODS most often present with a primary pulmonary disorder (eg, pneumonia, aspiration, lung contusion, near-drowning, chronic obstructive pulmonary disease exacerbation, hemorrhage, or pulmonary embolism). In the second, less common, form of MODS, the presentation is quite different. Patients affected by this form often have an inciting source of sepsis in organs other than the lung; the most common sources are intra-abdominal sepsis, extensive blood loss, pancreatitis, and vascular catastrophes.
In most patients with sepsis, a source of infection can be identified. The exceptions are patients who are immunocompromised with neutropenia, in whom an obvious source often is not found. Respiratory tract and abdominal infections are the most frequent causes of sepsis, followed by urinary tract and soft tissue infections.
For more on the etiology and epidemiology of sepsis, read here.
Q2: Which of the following is accurate about the presentation and physical examination of sepsis?
A2: In the early stages of sepsis, cardiac output is well-maintained or even increased
 Pay attention to the patient's skin color and temperature. Pallor or grayish or mottled skin are signs of poor tissue perfusion seen in septic shock. In the early stages of sepsis, cardiac output is well maintained or even increased. The vasodilation may result in warm skin, warm extremities, and normal capillary refill (warm shock). As sepsis progresses, stroke volume and cardiac output fall. The patients begin to manifest the signs of poor perfusion, including cool skin, cool extremities, and delayed capillary refill (cold shock).
Pay attention to the patient's skin color and temperature. Pallor or grayish or mottled skin are signs of poor tissue perfusion seen in septic shock. In the early stages of sepsis, cardiac output is well maintained or even increased. The vasodilation may result in warm skin, warm extremities, and normal capillary refill (warm shock). As sepsis progresses, stroke volume and cardiac output fall. The patients begin to manifest the signs of poor perfusion, including cool skin, cool extremities, and delayed capillary refill (cold shock).
Fever is a common symptom, though it may be absent in elderly or immunosuppressed patients. The hypothalamus resets in sepsis, so that heat production and heat loss are balanced in favor of a higher temperature. An inquiry should be made about fever onset (abrupt or gradual), duration, and maximal temperature. These features have been associated with increased infectious burden and severity of illness. However, fever alone is an insensitive indicator of sepsis; in fact, hypothermia is more predictive of illness severity and death.
Tachypnea is a common and often underappreciated feature of sepsis. It is an indicator of pulmonary dysfunction and is commonly found in pneumonia and ARDS, both of which are associated with increased mortality in sepsis.
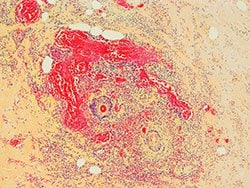
The frequency of ARDS in sepsis has been reported to range from 18% to 38% (with gram-negative sepsis, from 18% to 25%). The severity of ARDS may range from mild lung injury to severe respiratory failure. The onset of ARDS usually is within 12-48 hours of the inciting event. The patients demonstrate severe dyspnea at rest, tachypnea, and hypoxemia; anxiety and agitation are also present.
For more on the presentation and physical examination of patients with sepsis, read here.
Q3: Which of the following is accurate regarding the workup of sepsis?
A3: Urinalysis and urine culture are indicated for every patient who is in a septic state
 Urinalysis and urine culture are indicated for every patient who is in a septic state. Urinary tract infection is a common source for sepsis, especially in elderly individuals. Adults who are febrile without localizing symptoms or signs have a 10%-15% incidence of occult urinary tract infection. Obtaining a culture is important for isolating a specified organism and tailoring antibiotic therapy.
Urinalysis and urine culture are indicated for every patient who is in a septic state. Urinary tract infection is a common source for sepsis, especially in elderly individuals. Adults who are febrile without localizing symptoms or signs have a 10%-15% incidence of occult urinary tract infection. Obtaining a culture is important for isolating a specified organism and tailoring antibiotic therapy.
ACTH stimulation test is not recommended for identifying the subset of patients with septic shock or ARDS who should receive corticosteroid therapy. The American College of Critical Care Medicine does not recommend the routine use of free cortisol measurements in critically ill patients. No clear parameters for the normal range of free cortisol in such patients are recognized, and the free cortisol assay is not widely available, despite its advantages over the total serum cortisol assay.
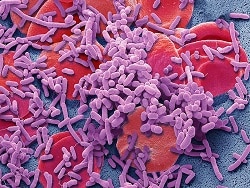
Although Gram staining may be helpful for identifying healthcare-related infections (eg, presence of yeast), it has not proved to be of clinical value in community-acquired intra-abdominal infections.
For more on the workup of sepsis, read here.
Q4: Which of the following is accurate regarding imaging studies used in patients with sepsis or suspected sepsis?
A4: If clinical suspicion of necrotizing fasciitis is high, a surgical consultation should be obtained immediately, often without imaging
 If clinical suspicion of necrotizing fasciitis is high, a surgical consultation should be obtained immediately, and the patient should be taken promptly to the operating room for intervention, often without the need for any imaging. CT and MRI cannot be relied on to make this diagnosis.
If clinical suspicion of necrotizing fasciitis is high, a surgical consultation should be obtained immediately, and the patient should be taken promptly to the operating room for intervention, often without the need for any imaging. CT and MRI cannot be relied on to make this diagnosis.
Chest radiography detects infiltrates in about 5% of febrile adults without localizing signs of infection; accordingly, it should be routine in adults who are febrile without localizing symptoms or signs and in patients who are febrile with neutropenia and without pulmonary symptoms. Chest radiography is useful in detecting radiographic evidence of ARDS, which carries a high mortality. The discovery of such evidence on a chest x-ray should prompt consideration of early intubation and mechanical ventilation, even if the patient has not yet shown signs of overt respiratory distress.
In adult patients with suspected intra-abdominal infection who are not undergoing immediate laparotomy, CT scanning of the abdomen is preferable to abdominal radiography. CT is the imaging modality of choice for excluding an intra-abdominal abscess or a retroperitoneal source of infection. Obesity or the presence of excessive intestinal gas markedly interferes with abdominal imaging by ultrasonography; therefore, CT is preferred in this setting.
For more on imaging studies in patients with sepsis, read here.