ORIGINAL ARTICLE
Timing of Renal-Replacement Therapy in Patients with Acute Kidney Injury and Sepsis
Saber D. Barbar, Raphaël Clere-Jehl, Abderrahmane Bourredjem, et al
N Engl J Med 2018; 379:1431-1442
DOI: 10.1056/NEJMoa1803213
Abstract
BACKGROUND 背景
Acute kidney injury is the most frequent complication in patients with septic shock and is an independent risk factor for death. Although renal-replacement therapy is the standard of care for severe acute kidney injury, the ideal time for initiation remains controversial.
急性肾损伤是感染性休克患者最常见的并发症,且是死亡的独立危险因素。尽管肾脏替代治疗是严重急性肾损伤的标准治疗,但理想的治疗时机仍存在争议。
METHODS 方法
In a multicenter, randomized, controlled trial, we assigned patients with early-stage septic shock who had severe acute kidney injury at the failure stage of the risk, injury, failure, loss, and end-stage kidney disease (RIFLE) classification system but without life-threatening complications related to acute kidney injury to receive renal-replacement therapy either within 12 hours after documentation of failure-stage acute kidney injury (early strategy) or after a delay of 48 hours if renal recovery had not occurred (delayed strategy). The failure stage of the RIFLE classification system is characterized by a serum creatinine level 3 times the baseline level (or ≥4 mg per deciliter with a rapid increase of ≥0.5 mg per deciliter), urine output less than 0.3 ml per kilogram of body weight per hour for 24 hours or longer, or anuria for at least 12 hours. The primary outcome was death at 90 days.
在这项多中心、随机、对照临床试验中,我们将早期感染性休克伴随严重急性肾损伤(RIFLE标准的衰竭阶段,但不伴有急性肾损伤的致命性并发症)的患者分组,即记录衰竭阶段后12小时内开始接受肾脏替代治疗(早期策略)或肾功能不恢复者延迟48小时开始治疗(延迟策略)。RIFLE标准的衰竭阶段指血清肌酐水平为基线的3倍(或 ≥4 mg/dl且迅速升高 ≥0.5 mg/dl),尿量< 0.3 ml/kg/h持续至少24小时,或无尿持续至少12小时。主要预后指标为90天病死率。
RESULTS 结果
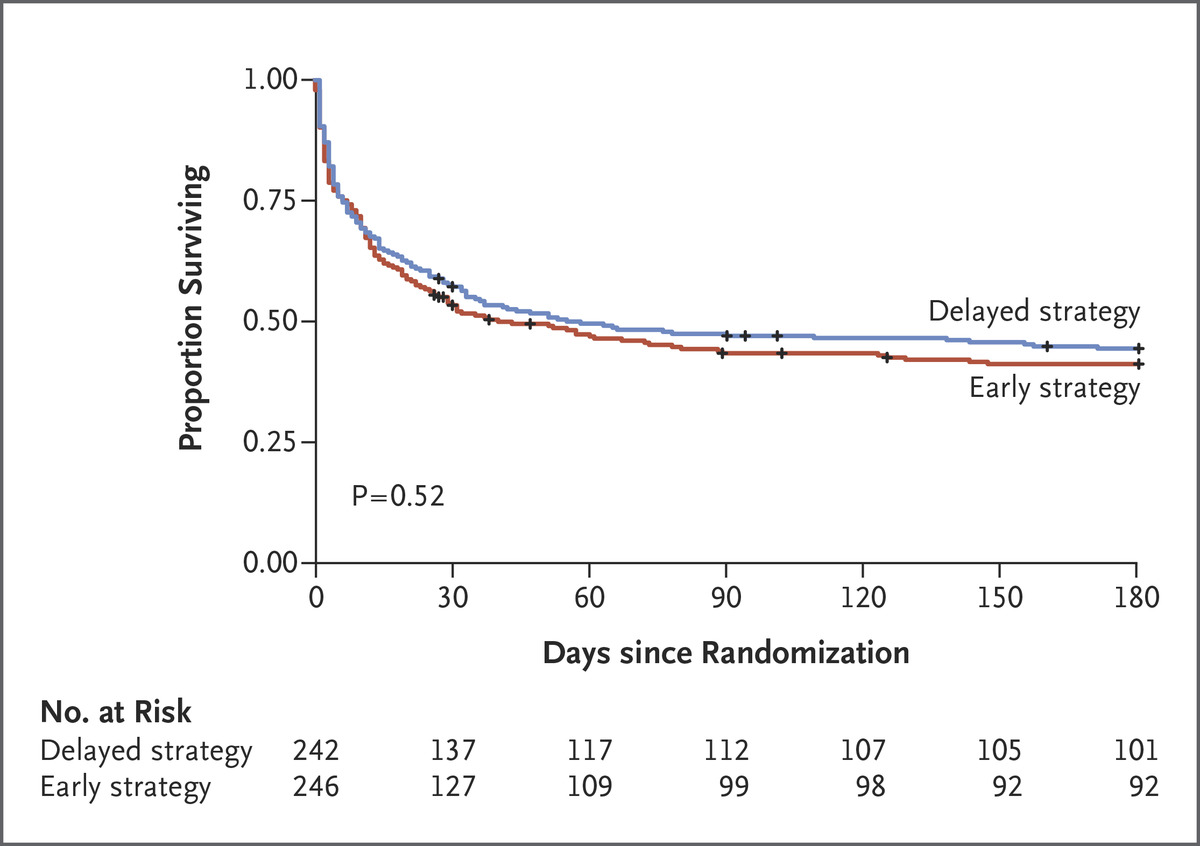
The trial was stopped early for futility after the second planned interim analysis. A total of 488 patients underwent randomization; there were no significant between-group differences in the characteristics at baseline. Among the 477 patients for whom follow-up data at 90 days were available, 58% of the patients in the early-strategy group (138 of 239 patients) and 54% in the delayed-strategy group (128 of 238 patients) had died (P=0.38). In the delayed-strategy group, 38% (93 patients) did not receive renal-replacement therapy. Criteria for emergency renal-replacement therapy were met in 17% of the patients in the delayed-strategy group (41 patients).
在计划中的第二次中期分析后,因治疗无效,研究终止。共有488名患者接受随机分组;两组患者基线特征没有显著差异。在477名90天随访资料完整的患者中,早期策略组58% (138/239)及延迟策略组54% (128/238)死亡(P=0.38)。在延迟策略组,38%(93名患者)未接受肾脏替代治疗。延迟治疗组17%的患者(41名)满足急诊进行肾脏替代治疗的标准。
CONCLUSIONS 结论
Among patients with septic shock who had severe acute kidney injury, there was no significant difference in overall mortality at 90 days between patients who were assigned to an early strategy for the initiation of renal-replacement therapy and those who were assigned to a delayed strategy.
对于伴随严重急性肾损伤的感染性休克患者,早期开始肾脏替代治疗策略与延迟开始的患者90天病死率无显著差异。
(Funded by the French Ministry of Health; IDEAL-ICU ClinicalTrials.gov number, NCT01682590.)