Greg Martin, MD
October 27, 2017
Angiotensin II for the Treatment of Vasodilatory Shock
Khanna A, English SW, Wang XS, et al; ATHOS-3 Investigators
N Engl J Med. 2017; 377:419-430
Background 背景
Septic shock occurs in the United States in approximately 200,000 people each year and leads to approximately 50,000 deaths,[1] and sepsis overall leads to approximately 1 in every 2-3 hospital deaths.[2] For patients with shock, fluid therapy is partially effective, but the cornerstone of pharmacologic therapy is use of vasopressors to mitigate the vasodilatory state.
在美国,每年约有200,000人发生感染性休克,其中50,000人死亡。而且,全身性感染导致的死亡占住院死亡患者的1/2到1/3。对于休克患者,液体治疗仅部分有效,使用升压药物减轻血管扩张是药物治疗的关键。
The most common vasopressors are catecholaminergic drugs, such as norepinephrine, epinephrine, phenylephrine, and dopamine. More recently, vasopressin has become available for patients with septic shock and recommended as a second-line agent for shock refractory to norepinephrine.[3,4]
最常用的升压药物为儿茶酚胺类药物,如去甲肾上腺素、肾上腺素、苯肾上腺素和多巴胺。近期,血管加压素逐渐用于感染性休克患者的治疗,且被推荐为对于去甲肾上腺素耐药的休克患者的二线治疗药物。
Study Summary 研究总结
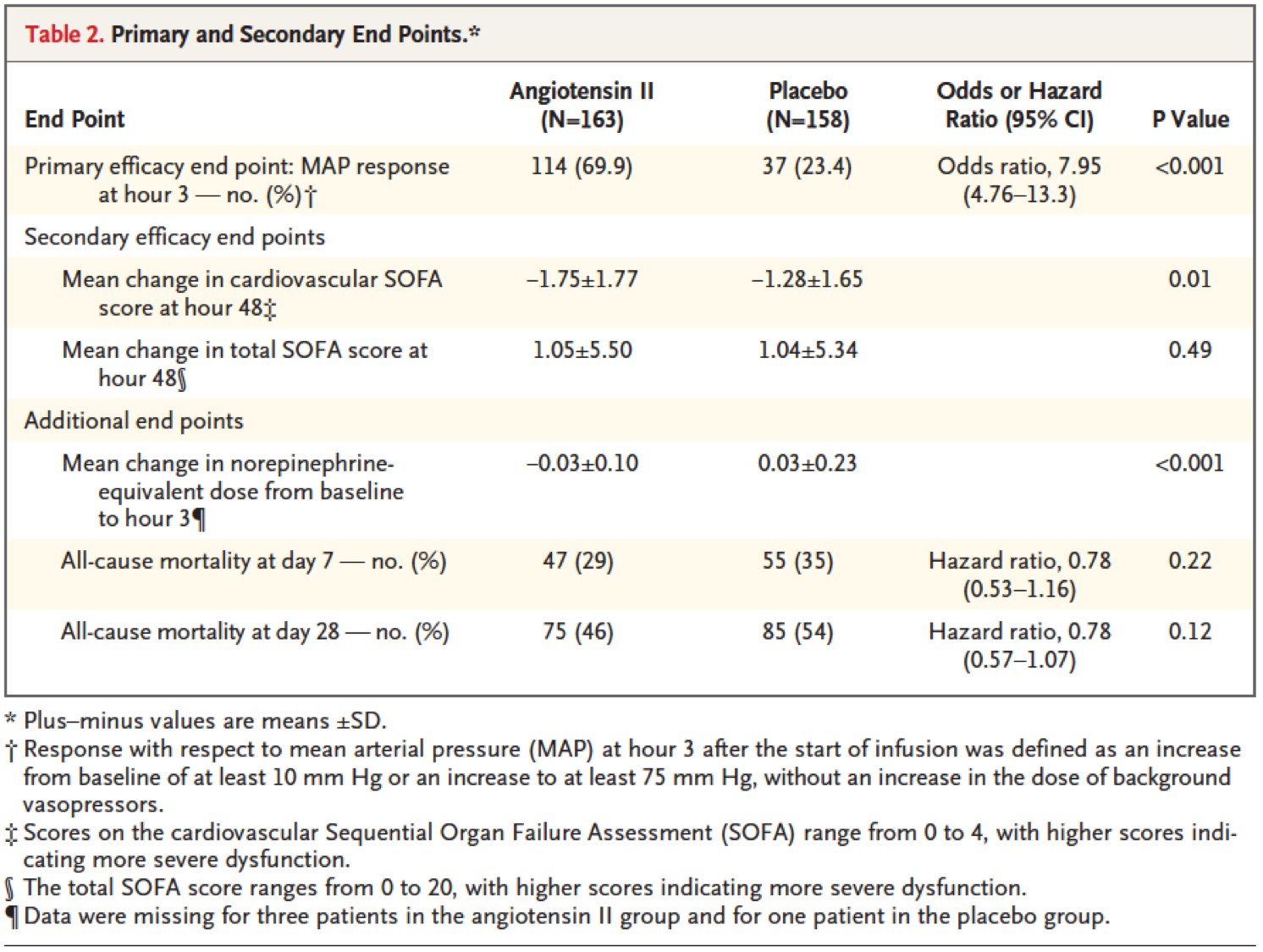
The authors of this study sought to determine the effectiveness of angiotensin II for blood pressure support in septic shock. They conducted a prospective, randomized clinical trial of 321 patients, comparing angiotensin II with placebo for the primary end point of a rise in mean arterial pressure of at least 10 mm Hg or to at least 75 mm Hg within 3 hours.
研究作者试图确定血管紧张素II对于感染性休克患者维持血压的效果。他们进行了一项前瞻随机临床试验,入选321名患者,比较了血管紧张素II与安慰剂的效果,主要预后终点为3个小时内平均动脉压升高至少10 mmHg或至少为75 mmHg。
More patients in the angiotensin II group than the placebo group reached the primary endpoint (114 of 163 patients [69.9%] vs 37 of 158 patients [23.4 %], respectively; P < .001). The cardiovascular Sequential Organ Failure Assessment score decreased more in the angiotensin II group at 48 hours than in the placebo group (−1.75 vs −1.28 ; P = .01). Serious adverse events and adverse events leading to drug discontinuation were modestly fewer (but not statistically significantly less) in the patients in the angiotensin II group. Death by day 28 was similar between groups (46% vs 54 %; P = .12).
与安慰剂组相比,血管紧张素II组更多患者达到主要终点 (114/163 [69.9%] vs 37/158 [23.4 %]; P < .001)。48小时后血管紧张素II组心血管系统SOFA评分下降更多(−1.75 vs −1.28 ; P = .01)。血管紧张素II组导致停药的严重不良事件稍微减少(但没有统计学差异)。两组患者28天病死率相似(46% vs 54 %; P = .12)。
The authors concluded that angiotensin II effectively increases blood pressure in patients with septic shock who did not respond to high doses of conventional vasopressors.
作者得出结论,感染性休克患者使用大剂量传统升压药物无效时,血管紧张素II能够有效提高血压。
Viewpoint 观点
This is an exciting and straightforward clinical trial of a new pharmacologic agent to increase blood pressure in vasodilatory shock. The study has limitations, however.
这是一项令人兴奋的临床试验,研究验证了一种新的药物能够提高血管舒张性休克患者的血压。然而,这项研究也存在局限性。
First, it was not sufficiently large to characterize all of the potential adverse effects or demonstrate an effect on mortality. However, the adverse event rates and mortality rates favored angiotensin II over placebo, suggesting a favorable risk/benefit assessment. Similarly, the study did not follow patients long-term to determine whether the drug may have adverse (or beneficial) effects on chronic organ dysfunction, recovery from critical illness, or long-term survival. And finally, as the authors pointed out, the active drug was more likely than placebo to result in a dose reduction in the conventional vasopressors being used for the patient, which would effectively unmask the providers as to whether the patient was receiving angiotensin II.
首先,研究样本量较小,不足以反映所有可能的不良反应,或显示对病死率的影响。但是,血管紧张素II组不良事件发生率及病死率较低,提示血管紧张素II的风险效益比较好。与此相似,研究没有对患者进行长期随访,从而无法确定药物对于慢性器官功能障碍、危重病康复或长期存活是否有不良或有益作用。最后,正如作者指出,与安慰剂相比,使用血管紧张素II更容易导致患者使用的传统升压药物剂量降低,这可能造成医务人员明确患者是否使用血管紧张素II。
With these caveats, the results are awaiting US Food and Drug Administration consideration for approval of the drug for routine clinical use in the United States. This would add to the armamentarium for patients with shock, which includes conventional catecholamine-based vasopressors and inotropes, and vasopressin.
尽管存在上述缺点,研究结果仍在等待FDA批准该药在美国进入常规临床应用。这样将在原有传统药物(儿茶酚胺类升压药物及强心药物和血管加压素)的基础上,增加我们治疗休克患者的药物选择。
How these will fit into practice guidelines and be coordinated in clinical practice remains to be seen. In addition, more studies with angiotensin II may be useful to understand its effect on lung edema, for example, given the known role of angiotensin in salt and water homeostasis.
尚不清楚血管紧张素II能否得到临床实践指南的推荐,或在临床实践中如何应用。另外,由于已知血管紧张素对水盐稳态的作用,更多研究可能有助于了解该药对于肺水肿的影响。
Abstract
References
1. Seymour CW, Rosengart MR. Septic shock: advances in diagnosis and treatment. JAMA. 2015; 314:708-717. Abstract
2. Liu V, Escobar GJ, Greene JD, et al. Hospital deaths in patients with sepsis from 2 independent cohorts. JAMA. 2014;312:90-92. Abstract
3. Surviving Sepsis Campaign. www.survivingsepsis.com Accessed October 11, 2017.
4. Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43:304-377. Abstract